Wednesday, February 26, 2020
Wednesday, February 19, 2020
Lupine Publishers: Lupine publishers | Modern Tools and Techniques fo...
Lupine Publishers: Lupine publishers | Modern Tools and Techniques fo...: Lupine Publishers | Agriculture Open Access Journal Introduction Soil salinity and brackish ground water are primary concerns for r...
Tuesday, February 18, 2020
Lupine Publishers: Lupine publishers | Modern Tools and Techniques fo...
Lupine Publishers: Lupine publishers | Modern Tools and Techniques fo...: Lupine Publishers | Agriculture Open Access Journal Introduction Soil salinity and brackish ground water are primary concerns for r...
Monday, February 17, 2020
Lupine Publishers: Lupine Publishers | Allegric Rhinitis: Pearls of W...
Lupine Publishers: Lupine Publishers | Allegric Rhinitis: Pearls of W...: Lupine Publishers | Journal of Otolaryngology High Impact Factor Abstract Statement of The Problem This provides an ove...
Sunday, February 16, 2020
Lupine Publishers: Lupine Publishers | The Prevention and Treatment o...
Lupine Publishers: Lupine Publishers | The Prevention and Treatment o...: Lupine Publishers | Open Access Journal of Complementary & Alternative Medicine Abstract Native people in West...
Lupine Publishers | Martial Arts as a Mindfulness in Motion: A Neurocognitive View
Lupine Publishers | Clinical Microbiology Reviews
Introduction
Mindfulness programs have given high visibility to bring the
impact of the practice through a well-structured protocol that can
be replicated over the years offering many clinical benefits as well
as a greater understanding of neurophysiological mechanisms
from immediate and long-term practice [1-5]. Since then, several
protocols have been created to give specificity to the public
suffering from mental health problems such as depression and
anxiety (MBSR, MBCT), addicts (MBRP), eating disorders (MBEAT),
pain and chronic illness (MBPM). With this, Mindfulness has
gained great popularity for a healthy population [6].
Thus, many studies have emphasized the structures and
neurophysiology that Mindfulness practice promotes [7-9]. Based
on these results, new protocols have been studied through body
movement. The basis is that the body becomes an excellent anchor
for maintaining attention, inasmuch attentional flexibility develops,
the attentional process becomes faster and more natural [10]. An
important factor in this finding is the main point that Mindfulness
neurophysiology integrates different areas at different times of
practice [11]. In the case of focused attention practice, attentional
neural networks are present until distraction occurs, where more
medial networks (default mode network) become more prominent
[12,13]. As this distraction comes out, a deeper network (salience
network) begins to activate so you can then decide to return to the
focused object [14,15].
This neural flow became known as the neurocognitive model
[11,14] that develops (neuroplasticity) throughout the training
(hours/year of practice) [16].
Therefore, Mindfulness is no longer understood only as a
practice of meditation or protocol but becomes a cognitive skill
or mental training that develops as these neural networks adjust
[17]. Then, body awareness is the starting point in the development
of Mindfulness due to sensory experience improves the focus
[18]. Thus, studies based on martial arts have been studied using
Mindfulness neurophysiology as a major aim [19,20]. Studies using
the Tai Chi Chuan [21] and Chi Kung [22] Mindfulness attitude had
a great impact on research, showing important neurophysiological
changes that corroborated with current findings that posterior
areas (parietal cortex) of the cortex play a key role in practitioners’
development [23-25]. Conscious movements have become a
practical way of training Mindfulness, while martial arts have
been an important way of maintaining these practices, considering
the synchronization of movement with the Mindfulness attitudes
described above.
Karate studies, for example, have gained prominence as training
develops cognitive aspects such as attention, working memory,
decision making [17,26,27]. The repetition of the movement
seems to be an important way to manage the cognitive skill in this
learning process, which is associated with a subtle recognition of
the movement [26] with lower activity of the brainpower [28,29]
and improved body balance [30]. Moreover, studies have shown
improvement in cognitive processing speed in older practitioners
[31] which related to neural efficiency [28,32]. More studies are
necessary to explore the efficacy of martial arts training in the
cognitive aspects, whereas Mindfulness has shown an important
factor to link the physical activity into cognitive abilities.
Read more Lupine
Publishers Blogger Articles Please Click on: https://lupinepublishers.blogspot.com/
Read more Lupine Biotechnology & Microbiology Journal Blogger articles please click on: https://lupine-biotechnology-microbiology.blogspot.com/
Wednesday, February 12, 2020
Lupine Publishers: Lupine Publishers | The Dynamics of Mounds-Cluster...
Lupine Publishers: Lupine Publishers | The Dynamics of Mounds-Cluster...: Lupine Publishers- Anthropological and Archaeological Sciences Journal Impact Factor Abstract Mounds are human made accumulation...
Tuesday, February 11, 2020
Lupine Publishers: Lupine Publishers | Varied clinical and Oral Prese...
Lupine Publishers: Lupine Publishers | Varied clinical and Oral Prese...: Lupine Publishers | Journal of Pediatric Dentistry Impact Factor Abstract Beckwith – Wiedemann syndrome is congenital, gen...
Monday, February 10, 2020
Lupine Publishers: Lupine Publishers | Somatic Mutations in Cancer-Fr...
Lupine Publishers: Lupine Publishers | Somatic Mutations in Cancer-Fr...: Lupine Publishers | Open Access Journal of Oncology and Medicine Abstract Somatic mutations have been perceived as the causal even...
Lupine Publishers | Post-Traumatic Stress Disorder: Symptoms, Screening and Treatment
Lupine Publishers | Microbiology Articles
Abstract
Sometimes,
as a result of experiencing or witnessing a distressful/traumatic event, there
are changes in the brain leading to an anxiety disorder called as Post
Traumatic Stress Disorder (PTSD). In the present article, symptoms of PTSD have
been described which may be categorized into four different categories viz.
flashbacks, avoiding behaviour, unusual alertness and negative feelings. Person
with PTSD has mental problems like depression, phobias and anxiety. Person when
feels that distressful event is occurring again or recalls in the memory, there
may be increased heart beats, high blood pressure etc. Here, screening for PTSD
has also been described. On MRI of brain, patient has difference in the size of
hippocampus compared to normal person. There are changes in the levels of
certain hormones involved in stress conditions also. Mostly doctors recommend
counselling, psychotherapy, medicines or combination of these.
Keywords:
Post traumatic stress disorder;
Traumatic events; Flashbacks; Depression; Anxiety; Hippocampus
Introduction
If
a person experiences or witnesses a traumatic event which is shocking, life
threatening, humiliating, distressful and feels helpless, these conditions may
happen in situations like crimes, fire, accident, death of a very loved person,
sexual or physical abuse in some form, rape, terrorist attack, ragging in the
college/ hostel etc. It causes changes in the brain leading to disturbance in
thinking and emotional process leading to an anxiety disorder called as
posttraumatic stress disorder (PTSD).
As
per an estimate, nearly 45 million people worldwide are suffering from PTSD.
This number may be even more since many people do not go to a doctor since they
do not realize about the seriousness of the situation or due to shame or societal
fear. It has also been predicted that women are more prone to PTSD than men
since men are generally more able to tolerate [1,2]. Generally, person gets
shocked and suffers from stress disorder within short span of the distressful
event, however, in some cases, symptoms develop at a later stage. It has been
found that with time, person instead of feeling better, he/ she feels worse and
becomes more anxious and fearful. In the present article, symptoms of the
disease have been discussed. Besides, clinical screening for diagnosis and
various treatment therapies and medicines available are discussed including
present trend of research for PTSD.
Symptoms
of PTSD
Generally,
symptoms are visible within three months of a distressful event, sometimes, it
takes longer. The symptoms of PTSD may be categorized into following four
categories, and one may develop either of these or jointly more than one
category.
Flashbacks/Intrusion
i.
The person has upsetting memories of the distressful event and generally sees
the event in nightmares feeling that the same event is occurring with him/her.
ii.
Person always feels as the traumatic (distressful) event will occur with
him/her again.
iii.
Person feels unusual body reactions like increased heart beats, high blood
pressure when he/ she feels that distressful event is occurring again or
recalls in the memory.
Avoiding behaviour
i.
Person avoids to go the place, or to meet the person(s), which reminds him/ her
of that distressful event. ii. Person avoids to discuss the event with anyone.
Unusual alertness
i.
Person behaves abnormally, for example, on ringing the telephone, he/ she
starts jumping or running towards the telephone.
ii.
Person develops the tendency to cause harm to himself/ herself or sometimes
even develops suicidal behaviour.
iii.
Person remains irritated all the time, unable to sleep properly, not able to
concentrate on any work.
Negative feelings
i.
Person feels unsafe everywhere.
ii.
Person develops persistent negativity and blames to himself/ herself for the
distressful event.
iii.
Person feels isolated/ detached from everyone.
iv.
Person feels reduced interest in life.
v.
Person has mental problems like depression, phobias and anxiety.
Although,
it is usual to feel anxiety immediately after the traumatic event but normally
there is healing with time. If healing did not occur with time and increased
with time, then these may be symptoms of PTSD.
American
Psychological Association (APA) has also formulated the guidelines for
detecting symptoms of PTSD. According to these guidelines, person has been
exposed to death or threatened death, serious injury or sexual violence whether
directly, through witnessing it, by it happening to a loved one, or during
professional duties. Besides, APA has also described more or less the same
symptoms as stated above [3,4]. It is advisable that if a person got witnessed
or suffered a distressful/ traumatic event and finds the persistent symptoms as
stated above for a longer time, he/she must visit expert doctor for checkup.
Physical
Symptoms
Besides,
person suffering from PTSD may also have following physical symptoms:
a)
observed that if behaviour changes persist for a longer time, person has
problems at work and in the When person is not able to sleep properly, he/ she
may feel much tiredness and other problems like body ache.
b)
Sometimes, person gets frequent infections. It is due to weakened immune
system.
c)
Besides, person may feel chest pain, stomach cramps/ pain, headache, dizziness
etc.
It
has also been marital relationship. Person starts drinking more alcohol or
taking drugs. Under the circumstances, it is advisable to get check up by an
expert doctor.
In case of children who suffer sexual abuse, may have
following visible symptoms:
a)
They generally have low self-confidence.
b)
They try to hurt themselves.
c)
Mostly appear sad, anxious, feared and prefer to stay in isolation.
d)
Sometimes become habitual for alcohol and/or drugs.
e)
They mostly behave aggressively.
f)
Sometimes, depending upon the age, show unusual sexual behaviour.
g)
Sometimes, depending upon the age, feel guilt and think, why he/ she did not
resist during the traumatic event; and afterwards have the feeling of taking
revenge.
h)
Sometimes, children exhibit reflection of the traumatic event in paintings,
plays, stories etc. They feel nightmares of traumatic event and get disturbed.
Due to fear, they hesitate to go to school or are not able to behave properly
with the friends. Sometimes, even are not able to study properly.
If
even a few symptoms are visible in a child who has witnessed or suffered any
sex abuse or other stressful event, parents without much delay must carry the
child to an expert doctor.
Screening
for PTSD
Doctors
generally give a screening test in order to confirm whether he/ she is
suffering from PTSD. If symptoms of PTSD get faded or disappear after a few
weeks or a couple of months, it may be acute stress disorder and not PTSD. If
person suffers from PTSD, symptoms are much severe and mostly appear after few
months of the distressful event. In case of PTSD, patient is likely to recover
within a year or so [5-7]. However, in some cases, patient suffers for years
with visible symptoms.
It
has been observed that some people suffer from PTSD after experiencing or
witnessing a traumatic event while others don’t.
There
are number of factors which increase the chances of PTSD like:
a.
If person does not get social support from the family or friends.
b.
If person in the past had some mental problems.
c.
If in the past, person experienced sexual abuse.
d.
If person’s physical health is weak.
e.
If after the tragedy, person got other problems too like firing from the job or
loss of some beloved one.
On the other hand, there may be conditions which help in not
developing PTSD. These are:
a. If person has emotional support from the friends/ family
members.
b. If person is having the quality to face the odd
situations boldly.
c. If person has the quality to cope up even under much
traumatic conditions.
According to some reports, genetic factors also influence
the condition by increasing depression, anxiety etc.
On MRI of brain, it has been found that people with PTSD
have difference in the size of hippocampus compared to normal individual since
this part of the brain is involved in processing emotions and memories which
may affect the flashbacks.
It has also been reported that levels of hormones which are released
under adverse conditions/ stress, has also been found to be different in
persons with PTSD compared to normal person.
Treatment
Mostly doctors recommend counselling, psychotherapy,
medicines or combination of these.
It is recommended that if talks are done repeatedly about
the traumatic event and about the fear present in the patient in a safe
environment, it may help to control the adverse thoughts. This therapy is
called Exposure Therapy. However, in this therapy, there is always a risk that
instead of improvement, condition of the patient may be worse.
Besides, person is convinced to think the whole event in a
new way. Psychotherapy may help in controlling the stress and fear.
Medicines
No patient must take any medicine without consulting a doctor.
If above mentioned treatments, exposure therapy and/or psychotherapy do not
work, Doctors normally prescribe selective serotonin reuptake inhibitors
(SSRIs) like paroxetine. The SSRIs help in reducing depression, anxiety and
sleep problems, symptoms mostly present in PTSD. However, sometimes,
antidepressant medicines have adverse effects like patient may think to
suicide. Some doctors also prescribe benzodiazepines for anxiety, sleep
problems, irritation etc. It is pertinent to mention that generally it must be
preferred not to give any medicine (unless there is a severe problem) since
these medicines only subsidize visible symptoms and person may become habitual
of taking these antidepressants.
Other
Therapies
1. Specialist asks the patient to recall the traumatic event
after making a specific type side to side eye movement. This therapy helps in
reducing the stress level for patients of PTSD and also helps in developing
positive emotions, thoughts, behaviour etc. This therapy is called as eye
movement desensitization and reprocessing.
2. It has also been suggested that if cortisol hormone
therapy is given to the patient just after the distressful event, it may help
in reducing the risk of PTSD.
3. Some doctors prefer to prescribe a recreational drug
which affects the memories more positively by encouraging a feeling of safety.
All these therapies are not proven therapies and require
more research.
Sareen [8] discussed important advances in PTSD considering
much increase in the number of patients of PTSD after many highprofile
traumatic events like wars in Iraq and Afghanistan, terrorist attacks of
September 11 on the World Trade Center. He reviewed the advances in the
diagnosis of PTSD, inclusion of its diagnosis in the Diagnostic and Statistical
Manual of Mental Disorders, impact of PTSD in the community, risk factors,
assessment and treatment.
Bisson et al. [2] emphasized on the need to know about PTSD.
According to them, responses to traumatic events vary depending upon the
individual and most of the persons do not suffer with any mental disorder after
traumatic event. Nearly 3% adults suffer from PTSD at any one time and ranging
from 1.9 to 8.8% people suffer lifetime. They also reviewed diagnosis and
treatment for the disease. They identified Cochrane and other relevant
systematic reviews, meta-analyses and other research papers. They also used
evidences from meta-analyses of randomized trials in writing the review
research article.
Shalev et al. [9] reviewed the clinical status of PTSD.
According to them, more than 70% humans experience a traumatic event at some or
other time in their lives, and 31% experience four or even more traumatic
events. PTSD is the most common psychopathological condition which has been
evidenced after experiencing traumatic events. They discussed symptoms of PTSD,
status of diagnosis, neurobiologic characters, treatments available and
clinical implications of the knowledge.
Dopfel et al. [4] reported individual variability in
behaviour and functional networks and mentioned that differences in
vulnerability to PTSD is due to predisposition or trauma exposure, is not
clear. They measured pre-trauma brain-wide neural circuit functional
connectivity, behavioural and corticosterone responses to trauma exposure, and
post trauma anxiety by using the predator scent model of PTSD in rats and a
longitudinal design. They showed that pre-existing circuit function can
predispose animals to differential fearful responses to threats.
Corbett et al. [3] showed that sphingosine-1-phosphate
receptor 3 in the medical prefrontal cortex of rats regulates resilience to
chronic social defeat stress. They also showed that sphingosine-1- phosphate
receptor 3 mRNA in blood of veterans with PTSD gets reduced when compared with
the combat exposed control subjects. They also negatively correlated the
expression of sphingosine-1- phosphate receptor 3 mRNA with the severity of the
symptoms. On the basis of results, they concluded that sphingosine-1-phosphate
receptor 3 is a regulator of stress resilience and sphingolipid receptors are
important substrates of relevance to stress related psychiatric disorders.
Holmes et al. [5] showed that synaptic loss and deficits in
functional connectivity may be considered as symptoms for major depressive
disorder (MDD) and PTSD. They also mentioned that synaptic vesicle glycoprotein
2A can be used to index the number of nerve terminals and that is an indirect
estimate of synaptic density. They showed that lower synaptic density is
associated with the severity of depression and network alterations. They
claimed that their study is the first to show in vivo evidence correlating
lower synaptic density with depression severity and network alterations. This
study may be helpful in treating depression.
Iribarren et al [6] reviewed the current knowledge of PTSD.
They emphasized for the role of allostasis in fundamental research on PTSD.
They also argued in support about the future of clinical and translational
research in PTSD and supported systematic evaluation of the research evidence in
treatment of the disease. They showed a strong correlation of novel sleep EEG
coherence markers with diagnosis and severity of PTSD. For this, they collected
overnight polysomnography data containing EEG across sleep and wake states of
many veterans with PTSD and without PTSD (for control). They calculated brain
coherence markers from EEG signals using a novel approach. They showed that EEG
based brain coherence markers can be used as an objective means for determining
the presence and severity of PTSD [10,11].
Conclusion
Post-traumatic stress disorder (PTSD) is a mental disease
which changes the life of the person. After some distressful event, if a
person’s behaviour changes and does not revert back within reasonable time,
person must consult a specialist doctor and proper treatment must be taken.
Although therapy commonly given may not cure completely, patient’s condition
may improve. There is requirement of more research on PTSD.
Acknowledgement
Author acknowledges the facilities of the Department of Biotechnology,
Ministry of Science and Technology, Government of India, New Delhi (DBT) under
the Bioinformatics Sub Centre as well as M.Sc. Biotechnology program used in
the present work.
Read more Lupine Publishers Blogger
Articles Please Click on: https://lupinepublishers.blogspot.com/Read
more Lupine Biotechnology& Microbiology Journal Blogger articles please click on: https://lupine-biotechnology-microbiology.blogspot.com/
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
Sunday, February 9, 2020
Lupine Publishers: Lupine Publishers: Lupine Publishers | Hamstring I...
Lupine Publishers: Lupine Publishers: Lupine Publishers | Hamstring I...: Lupine Publishers: Lupine Publishers | Hamstring Injuries in Taekwond... : Lupine Publishers | Journal of Orthopaedics Abstract ...
Thursday, February 6, 2020
Lupine Publishers: Lupine Publishers Scilit Indexing Journals
Lupine Publishers: Lupine Publishers Scilit Indexing Journals: Lupine Publishers Journals Lupine Publishers Scilit Indexing Journals Current...
Tuesday, February 4, 2020
Lupine Publishers: Lupine Publishers Scilit Indexing Journals
Lupine Publishers: Lupine Publishers Scilit Indexing Journals: Lupine Publishers Journals Lupine Publishers Scilit Indexing Journals Current...
Monday, February 3, 2020
Lupine Publishers: Lupine Publishers | Hamstring Injuries in Taekwond...
Lupine Publishers: Lupine Publishers | Hamstring Injuries in Taekwond...: Lupine Publishers | Journal of Orthopaedics Abstract Background: Hamstring injuries frequently occur in sports involving ex...
Lupine Publishers | Whole-Cell Assays for Discovering Novel Efflux Inhibitors for Use as Antibiotic Adjuvants
Lupine Publishers | Journal of Biotechnology
Abstract
Antimicrobial resistance (AMR) is a growing problem worldwide.
Resistance to antibiotics can occur in a number of ways, one
of which is removal of the drugs from the cell via efflux pump
macromolecular machineries. As such, efflux pumps can provide a
background level of resistance to many different classes of
antimicrobials and are a major contributor to AMR. Inhibition of efflux
pumps therefore has the potential to reverse resistance to many
antibiotics in one go and is an attractive potential for treating
resistant infections. Whilst a number of efflux inhibitors are known,
none are currently used clinically due to harmful side effects.
Development of novel inhibitors is therefore imperative. The article
aims to review accumulation assays and efflux assays, two of
the most common laboratory techniques used to identify and characterise
candidate efflux inhibitors.
Keywords:Efflux pumps; Efflux inhibitors; Efflux assays; Antimicrobial resistance; Drug discovery
Introduction
Globally, antimicrobial resistance is a rising public health
challenge. Particular infections including pneumonia, Tuberculosis
(TB), gonorrhoea, and salmonellosis are becoming more difficult
to treat. Of new TB cases, 3.5% are either resistant to rifampicin
(the most effective first line drug) or are multi-drug resistant,
rising to 18% for previously treated individuals [1] Furthermore,
there are fears that Neisseria gonorrhoeae has already developed
resistance to all currently recommended treatments [2]. There is
a desperate need for new antibiotics to treat these most resistant
of infections, but the huge costs, long timescale and high attrition
rate of drug discovery means that this is a slow process. Twenty
classes of antibiotics were discovered between 1940 and 1962,
yet only two have been developed since then [3]. Moreover, for
any novel antibiotic developed, it is likely that resistance will
quickly emerge once it is brought into clinical use, especially
with the frequent misuse of antibiotics which drives selection for
resistance. Therefore, other strategies must be taken in parallel to
antibiotic development, or there will be a continuous arms race of
drug development and resulting gain of resistance, a battle we are
currently losing.
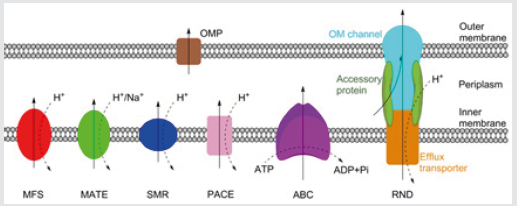
Figure 1: Schematic representation of the MFS, MATE, SMR,
PACE, ABC and RND families of bacterial efflux pumps, plus
an outer membrane protein channel (OPM), shown here in a Gram-negative
bacterium. RND family efflux pumps comprise
of a tripartite complex formed from an inner membrane efflux
transporter, an outer membrane channel, and a periplasmic
accessory protein. All six families, with the possible exception of the
PACE family, also have representatives in both Grampositive
and acid-fast bacteria. Bold arrows indicate the direction of drug
efflux, and dashed arrows show ion movement.
Antibiotic resistance can occur via acquired or intrinsic
mechanisms. Acquired resistance, typically via horizontal transfer
or spontaneous mutation, often functions by altering the drug
target or production of enzymes which degrade the antibiotic.
Acquired resistance, gained in response to antibiotic treatment, is
usually only effective against a single drug. Intrinsic resistance, on
the other hand, refers to the non-specific mechanisms of antibiotic
resistance evolved ancestrally, including the impermeable outer
membrane of Gram-negative or acid-fast group of bacteria, and
drug efflux pumps which remove drugs from the cell [4]. There are
currently six families of bacterial efflux pumps identified: the ATPBinding
Cassette (ABC) family, the Major Facilitator Superfamily
(MFS), the Multidrug And Toxin Extrusion (MATE) family, the Small
Multidrug Resistance (SMR) family, the Resistance-Nodulation-Cell
Division (RND) superfamily and the Proteobacterial Antimicrobial
Compound Efflux (PACE) family, which has not yet been structurally
characterised. The ABC family hydrolyse ATP directly to drive
efflux, whereas the other five utilise transmembrane ion gradients
[5]. Whereas the RND family directly effluxes antibiotics across
both membranes, the other five families only transport antibiotics
across the inner membrane. From the periplasm, drugs can exit the
cell via outer membrane protein channels or by entering the RND
complex (Figure 1).
Efflux pumps are often non-specific, and as such can provide
resistance to a wide range of antimicrobials. They have been
implicated in contributing towards the multi-drug resistant
phenotypes of Mycobacterium tuberculosis [6], Pseudomonas
aeruginosa [7], Neisseria gonorrhoeae [8], and Streptococcus
pneumoniae [9], amongst others. Inhibition of drug efflux is
therefore an exciting prospect for treating drug resistant bacteria
and may enable old antibiotics to re-enter clinical usage. There is
compelling evidence that the use of efflux pump inhibitors as an
adjuvant may aid treatment of resistant infections of many types
[6-12]. However, despite a number of potent efflux inhibitors
being known, none have entered clinical use. In most cases this is
because the compounds are toxic at the concentrations required
to inhibit efflux [13]. There is therefore a pressing need to develop
novel clinical efflux inhibitors. To achieve this, assays are needed
to validate the inhibitory activity of novel compounds. One way
this can be achieved is by using standard antibiotic susceptibility
testing, such as the resazurin-based microplate assay to determine
if the putative inhibitor, at sub-MIC concentrations, is able to lower
the MIC of a known antibiotic. This method has the benefit of being
relatively easy and high-throughput; furthermore, it is possible to
combine this method with mutants of efflux pumps to confirm that
the effect on the MIC is occurring specifically via inhibiting efflux,
and even to identify which efflux pump is inhibited [14]. However,
using reduction of MICs to identify and validate efflux inhibitors
is fairly insensitive, and so is of limited use. Only large changes
to efflux will likely have an effect on MICs, and so less potent
inhibitors may be dropped out. Furthermore, as this method does
not measure efflux, it is difficult to directly attribute changes in MIC
to efflux inhibition [15]
A more direct way is therefore needed to study the effect of
candidate inhibitors on efflux. One way is to follow the movement
of an efflux pump substrate, often a fluorescent molecule, into and
out of bacterial cells, and use this as a measure of efflux activity.
Many different molecules are used to measure efflux, with ethidium
bromide and Nile red being two of the most common. Ethidium
bromide fluoresces strongly when bound to DNA, and Nile red
fluoresces when in non-polar environments such as the membrane
[16,17]. This therefore gives these molecules the advantage that they
fluoresce differentially in extra- and intracellular environments,
providing a sensitive indication of rate of efflux from the cell, and
helping eliminate background fluorescence. These methods fall
into two main categories; those which follow the accumulation of
the molecule within the cell, and those which follow its efflux.
Accumulation Assays
Whilst there are variations, most accumulation assays typically
follow a similar procedure. At the start of the assay, there is no
dye added to the bacteria. This is then added to the reaction, and
its accumulation within the cells followed over time, typically by
measuring the fluorescence with dyes such as ethidium bromide.
Eventually, accumulation will tail off, with fluorescence reaching a
steady state. This reflects an equilibrium being achieved between
influx and efflux of the dye. This assay can be performed with added
efflux inhibitors [18]. By inhibiting efflux, more dye accumulates
within the cells compared to untreated ones, with steady state
being achieved at a higher fluorescence. This assay can therefore
be used as a very simple test to validate the inhibitory activity of
a candidate efflux inhibitor [19]. Similarly, accumulation assays
are often used to observe changes in efflux ability in knockout,
knockdown or overexpression mutants.
If a knockout/knockdown mutant accumulates more dye, it can
be assumed that the gene encoded a protein important for drug
efflux, or a regulator of these, and vice versa with overexpression
mutants. These two approaches can be combined, with different
mutants treated with efflux inhibitors to see if they have a greater
or lesser effect on dye accumulation than for wild-type cells. This
can help determine which efflux pump the inhibitor affects [7].
However, there are problems with using accumulation assays, the
most important being that accumulation is not a direct measure
of efflux. Rather, it reflects a number of factors, predominantly
the balance of influx and efflux rates. Influx depends greatly on
the permeability of bacterial membranes, which can vary greatly
between even closely related strains due to differing membrane
compositions [20]. Therefore, unless influx rates are known,
kinetic data cannot be obtained from accumulation assays and
results remain qualitative. Whilst this limits usage of accumulation
assays to comparisons between isogenic mutants, or groups treated
with different inhibitors, the assay remains a conclusive way to
determine if a molecule possesses inhibitory activity, and so is
frequently used to validate new efflux inhibitors.
Efflux Assays
If a quantitative measure of efflux is required, then a more
direct efflux assay should be used. This follows a similar premise to
accumulation assays, but instead involves preloading the cells with
dye and following its subsequent efflux. To achieve this, cells are
incubated with a dye or other efflux pump substrate, and a known
efflux inhibitor such as CCCP. This causes the dye to accumulate to a
maximum level. Then, the cells are washed to remove the inhibitor
and any remaining extracellular dye. The cells are then reenergised,
typically with glucose, which restarts efflux. The movement of the
dye out of the cells can be followed by recording the decreasing
fluorescence [15]. As this method is a direct measure of efflux, kinetic
data can be obtained for efflux rates, which allows comparisons to
be made more broadly, rather than just between isogenic species.
In much the same way as with accumulation assays, modifications
can be made to study the effects of putative inhibitors or different
mutations on efflux rates [12,21].
Efflux assays are very sensitive, and they allow for validation
and characterisation of novel inhibitors, which may potentially
have clinical usage. Whilst the efflux assay is widely used, it is not
always applicable. Non-fermenter bacteria, including Pseudomonas
and Acinetobacter, are unable to metabolise glucose, and so
cannot be easily reenergised. This means that efflux assays can be
unsuitable for some bacteria, and instead accumulation assays are
more commonly used [7,22].
Limitations with these Assays
A fundamental problem with both types of assay is that using
ethidium bromide or another dye to measure efflux or accumulation
is of limited clinical relevance, and may not reflect well the efflux of
any particular antibiotic. This can be due to the dye and antibiotic
having very different kinetics of efflux, and furthermore, they may
not even be substrates for the same efflux pumps. In addition, as
ethidium bromide intercalates with DNA, there is a lag time in efflux
in which it dissociates, followed potentially by a two-step efflux
mechanism in which it is first transported to the periplasm. This can
lead to underestimates of efflux rate, and so may be a poor reflection
of efflux rates of antibiotics [23]. Therefore, where possible, it is
better to use the antibiotic of interest itself as a direct measure of
efflux, although this tends to be far more difficult experimentally.
Certain antibiotics, such as fluroquinolones and tetracyclines have
endogenous fluorescence which enables their accumulation to be
followed [24]. For non-fluorescent antibiotics, Mass-Spectroscopy
(MS) can be used to directly study their accumulation. A recent
proposed joint protocol for spectrofluorimetric and MS analyses
suggests that the two methods are complementary and together can
accurately measure antibiotic accumulation, demonstrated with
fluroquinolones [25]. MS analyses, rather than spectrofluorometric,
may also provide a better way to screen natural compounds
for efflux inhibitory activity. Many natural compounds have
endogenous fluorescence, which can make it hard to isolate and
interpret fluorescence changes due to dye accumulation or efflux.
As before, the actual antibiotic, rather than a dye, could be used, and
MS used to determine how much accumulates with and without the
candidate inhibitor.
One of the biggest problems facing the development of novel
efflux inhibitors is the lack of high-throughput assays to validate
putative compounds. Whilst both the accumulation and efflux assays
are relatively easy to perform and can reliably confirm if inhibition
occurs, both are limited on throughput. Therefore, whilst some in
silico screening has been performed [26], limitations in throughput
have so far prevented large-scale screening of libraries in vitro.
Instead, the search for novel inhibitors has relied extensively on
prior knowledge to select candidates for validation. Whilst the hit
rate with this has been relatively high, the overall number of new
inhibitors found has been low, and it is rare to identify completely
novel inhibitors in this way. This is in part why no inhibitors have
made their way into clinical usage, as many are closely related and as
such are similarly toxic. Development of high-throughput screening
assays for novel inhibitors is therefore necessary if efflux inhibitors
are to progress clinically. Recently, the Back assay was developed,
which uses a 96-well plate format combined with MS. This was able
to test in triplicate 12 compounds at 4 concentrations each, for two
different Escherichia coli strains [27]. This progression to more
high-throughput screening is likely to be the driving force behind
development of novel efflux inhibitors, and further work needs to be
done to optimise assays before large scale-screening of compound
libraries can be performed. Ultimately, the development of clinical
efflux inhibitors used therapeutically as antibiotic adjuvants may
be what turns the tide in the battle against antibiotic resistance.
Acknowledgment
The authors would like to thank the British Society for
Antimicrobial Chemotherapy, without whose funding this work
would not have been possible. We also wish to thank Dr Arundhati
Maitra for her time and advice when writing the article, as well as
for help with ChemBioDraw
Read more Lupine Publishers Blogger Articles please click on: https://lupinepublishers.blogspot.com/
Read more Biotechnology & Microbiology Journal blogger articles please click on: https://lupine-biotechnology-microbiology.blogspot.com/
Subscribe to:
Comments (Atom)
FGFR Gene Mutation and Pfeiffer Syndrome
Abstract Pfeiffer syndrome is a genetic disease caused by a defect in the FGFR-1 or FGFR-2 genes. This syndrome affects the skeleton, whet...


